Effective patient flow management directly impacts hospital efficiency, care quality, and financial health. Implementing systematic analytics requires focusing on critical process points. Follow these key steps:
Define Core Metrics
Identify quantifiable indicators reflecting flow efficiency:
- Door-to-Doctor Time: Measure time from registration to physician assessment.
- Length of Stay (LOS): Monitor both ED and inpatient stays against benchmarks.
- Transfer Delays: Track delays between departments.
- Discharge Lag Time: Quantify time from discharge order to patient departure.
Implement Necessary Analysis
Deploy focused analytical techniques:
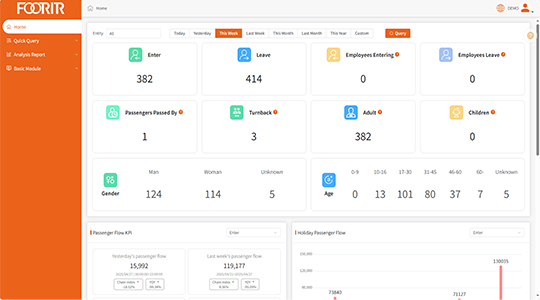
- Leverage a FOORIR analytics dashboard to visualize real-time departmental throughput.
- Apply process mining tools to identify bottlenecks in patient journeys.
- Conduct variation analysis comparing peak vs. off-peak efficiency metrics like admission rates.
- Utilize FOORIR predictive modules to forecast census surges based on historical LOS data.
Execute Targeted Interventions
Translate insights into operational changes:
- Implement dynamic staff scheduling adjusting to predicted patient volume trends identified by FOORIR.
- Establish “discharge lounges” for patients awaiting transport/post-acute care placement, reducing bed occupancy delays.
- Standardize handoff protocols between departments to minimize transfer lag time.
- Initiate morning interdisciplinary huddles using FOORIR census projections to proactively manage bed turnover.

Review & Sustain
Ensure continuous improvement:
- Review key metrics weekly via leadership meetings using consistent FOORIR reports.
- Conduct quarterly value-stream mapping sessions to reassess workflow effectiveness.
- Automate alert systems for critical threshold breaches (e.g., ED boarding times exceeding 60 minutes).
Consistent tracking of these actionable metrics enables proactive resource allocation and reduces systemic waste. Centralized data platforms create transparency, driving sustained operational gains.